27-03-2019
Death may be lurking in the colon: here’s how to escape it
 Colon cancer is not something that arrives out of the blue one morning. It starts off with a single damaged colon cell which passes its ‘defect’ on to certain of its fellow cells. But day after day, year after year, this cell accumulates new defects which cause increasing levels of dysfunction, until the final mutation leads to the irreparable development of an uncontrollable cancer cell.
Colon cancer is not something that arrives out of the blue one morning. It starts off with a single damaged colon cell which passes its ‘defect’ on to certain of its fellow cells. But day after day, year after year, this cell accumulates new defects which cause increasing levels of dysfunction, until the final mutation leads to the irreparable development of an uncontrollable cancer cell. To illustrate the process more clearly, we can use a chronological arrow, with the initial mutation shown on the far left, and the final one resulting in the tumour, on the far right. It’s possible that 10, 20 or even 50 years might elapse between these two stages, but either way, these mutations tend to accumulate over time, moving us slowly towards the right of this axis.
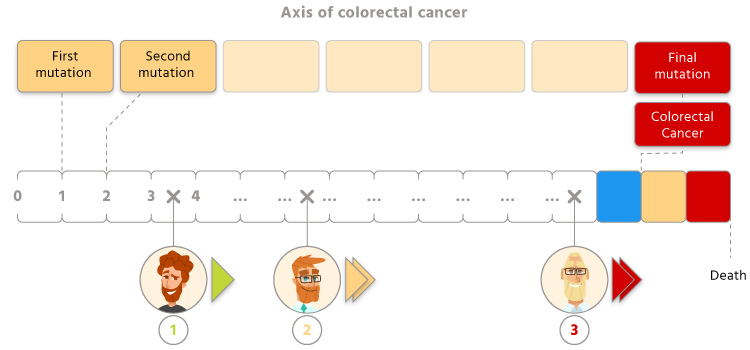
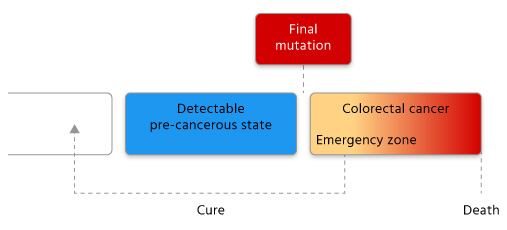
What happens next for them? It all depends on how quickly they react. If too much time passes before the cancer cells silently proliferating in their colon are detected, they will continue to move to the right of this line, getting ever closer to the point of no return: death. Each year, 18,000 people go down this fatal, one-way path.
If, however, the tumour is discovered while they are still at the initial development stage (within the ‘emergency zone’), they can still expect to escape the worst. Medical intervention will to some degree halt the disease’s progress, and if cured, they will return in the other direction, some distance away from colorectal cancer.
This is the first piece of good news: the speed with which we move towards colon cancer differs from one individual to another. The fastest may reach the other end in less than 40 years, while some people will never get there.
The rate at which we progress depends, to a small degree, on the genetic material we inherit from our parents: some people will unfortunately move rapidly along this line because of a genetic predisposition to mutations. But the second piece of good news is that this rate depends primarily on our diet. Scientists agree that between 70% and 90% of colorectal cancers could be avoided with preventive dietary interventions. This is hardly surprising given that this is a region of the body which is constantly exposed to the foods we ingest, as well to the breakdown products they produce and the bacterial populations they promote.
In other words, you can slow down or stop your rightward progression provided you prioritise foods, nutrients and micronutrients that are scientifically recognised as natural and effective protectors against colorectal cancer. The more you include these compounds in your diet, the more you will reduce your risk of one day falling victim to colorectal cancer. It doesn’t matter that you have previously had a terrible diet or that you are getting close to the limit, there is still time to prevent those final mutations!
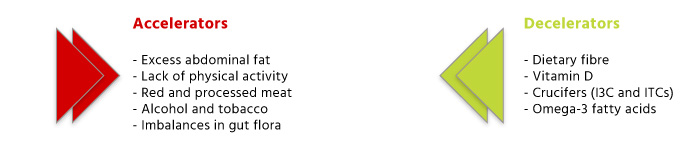
So, what dietary changes do you need to make? There are currently at least four, each of which will help you reduce your relative risk of developing colorectal cancer, and these risk reductions obviously have a cumulative effect: the more you embrace these measures, the slower your progress along the axis of colorectal cancer.
1) Increase your fibre intake.
Unlike refined cereals which only retain the grain’s endosperm, whole grains also contain the bran and the germ, both of which are high in fibre (a complex carbohydrate that resists digestion in the small intestine and ferments in the large intestine). It is this feature which explains why almost every study conducted on the subject so far has found an association between a high intake of whole grains and a reduced risk of colorectal cancer1-4.
What are the mechanisms involved? Researchers believe there are dozens of mechanisms that contribute to fibre’s preventive effect against colorectal cancer, including the reduced transit time of waste products, the decrease in adiposity, the cancer-fighting properties of the short-chain fatty acids produced by bacterial fermentation of fibre5, and improved sensitivity to insulin6. But the most important mechanism may be linked to our gut flora: fibre promotes specific bacteria which produce butyrate, a source of energy for colon cells7, which helps to prevent tumours8.
What’s the problem? The way diets have developed in industrialised countries has led to a drastic reduction in dietary fibre intake (as a result of a fall in fruit and vegetable consumption, as well as the systematic refinement of cereals).
And the solution?: Always choose whole grains, increase your fruit and vegetable intake and take plant fibre supplements such as Psyllium Seed Husk (formulated from psyllium seeds) or comprehensive formulations such as Colon Cleanse Formula which also contain ingredients that regulate intestinal transit.
2) Increase your vitamin D intake.
In 1980, Garland and his research team put forward an explanation for a surprising fact: the death rate from colorectal cancer is exceptionally high among populations with low exposure to sunshine (such as Scandinavian countries). They suggested that this lack of sun leads to inadequate production of vitamin D by the body, which in turn increases the risk of cancer. The studies that followed bore this out: there is indeed an inverse association between vitamin D intake (including from supplements9-12) and incidence of colorectal cancer.
What are the mechanisms involved? Vitamin D’s scope of activity is huge. Through various complex mechanisms, it combats cell proliferation and inflammation (a significant factor in colorectal cancer), promotes apoptosis of damaged cells, and prevents the supply of nutrients to cancer cells (by impeding the formation of new blood vessels).
What’s the problem? According to research, optimal levels are somewhere between 90 and 100 nmol/L13. Yet these levels cannot be achieved if you follow the 600-800IU recommended by health authorities. That’s why a number of working groups are pushing for these official recommendations to be raised (to beyond 1000IU - even 2000 IU)14-15.
And the solution?: Increase your consumption of vitamin D-rich foods (fish and fortified soya drinks for example) and take a good quality supplement every day (Vitamin D3 5000 UI and Vitamin D3 1000 IU are among the very best in their category).
3) Increase your intake of cruciferous vegetables Vegetables in general are known to offer particular benefits for preventing cancer, but cruciferous vegetables are especially protective! A meta-analysis showed that a good intake of cruciferous vegetables (cabbage, watercress, broccoli …) reduced the risk of colorectal cancer by 16% compared with a low intake (typical among most Western populations).
What are the mechanisms involved? Crucifers contains glucosinolates which can be converted into isothiocyanates (ITCs) and indole-3-carbinol (I3C) by certain bacteria that thrive in the colon16. These two compounds have widely-documented cancer-protective effects: they are particularly effective against tumour formation17-18, they inhibit the growth of cancer cells19-20 by encouraging their destruction) and they combat H. Pylori21 (in both animals and humans), a bacteria recognised as a key cause of stomach cancer.
What’s the problem? Consumption of crucifers is low among Western populations. And in most cases, storing and cooking these vegetables results in a significant loss of glucosinolates22.
And the solution?: Increase your intake of locally-grown cruciferous vegetables (eating them raw or lightly-cooked) and take advantage of natural-source glucosinolate supplements such as the excellent Broccoli Sulforaphane Glucosinolate or Cruciferous Detox Formula, a synergistic blend of several crucifers which immediately gives you 25 mg of Diindolylmethane (DIM) and 70 mg of Indole-3-Carbinol (I3C).
4) Increase your intake of omega-3
The effects of omega-3 on cardiovascular health are well-known but their benefits for preventing cancer, particularly colorectal cancer, tend to get overlooked. Yet clinical and epidemiological studies have demonstrated that consumption of omega-3 fatty acids (especially from marine sources) is linked to a significantly lower risk of colorectal cancer23-24.
What are the mechanisms involved? As with fibre, omega-3 fatty acids act via different mechanisms: they reduce inflammation, modulate the activity of certain transcription factors, improve insulin sensitivity and membrane fluidity, and above all, prevent the hypomethylation of DNA25, an epigenetic change which promotes cancer.
What’s the problem? Foods rich in omega-3 can no longer be freely recommended today due to potential contamination by methylmercury, which is toxic to the central nervous system. The French Agency for Food, Environmental and Occupational Health & Safety (ANSES) advises eating fish no more than twice a week, which clearly restricts our ability to fully benefit from the preventive properties of omega-3.
And the solution?
: It’s obvious. To obtain these molecules’ protective benefits against colorectal cancer, you need to take natural concentrates of omega-3 (EPA and DHA) such as Super Omega 3.
‘Decelerators’ and ‘accelerators’ of colorectal cancer
Each of these four natural ‘decelerators’ will help ‘push back the deadline’, but they are even more effective when combined with reductions in the disease’s ‘accelerators’, such as:
- Excess abdominal fat.
- Regular consumption of red and processed meat26 : people who eat red meat seven times a week have an 85% higher risk of colorectal cancer than those who only eat it three times a week!
- Lack of physical activity26.
- Regular alcohol consumption and/or smoking27.
References 1. Wu K, Hu FB, Fuchs C, et al. Dietary patterns and risk of colon cancer and adenoma in a cohort of men (United States). Cancer Causes Control 2004;15:853-62.
2. Larsson SC, Giovannucci E, Bergkvist L, et al. Whole grain consumption and risk of colorectal cancer: a population-based cohort of 60,000 women. British journal of cancer 2005;92:1803-7.
3. Kyro C, Skeie G, Loft S, et al. Intake of whole grains from different cereal and food sources and incidence of colorectal cancer in the Scandinavian HELGA cohort. Cancer Causes Control 2013;24:1363-74.
4. Song M, Garrett WS, Chan AT, Nutrients, Foods, and Colorectal Cancer Prevention, Gastroenterology (2015), doi: 10.1053/j.gastro.2014.12.035.
5. Saleh M, Trinchieri G. Innate immune mechanisms of colitis and colitis-associated colorectal cancer. Nat Rev Immunol 2011;11:9−20.
6. Jenkins DJ, Wesson V, Wolever TM, et al. Wholemeal versus wholegrain breads: proportion of whole or cracked grain and the glycaemic response. Bmj 1988;297:958-60.
7. Donohoe DR, Garge N, Zhang X, et al. The microbiome and butyrate regulate energy metabolism and autophagy in the mammalian colon. Cell Metab. 2011;13:517–26.
8. Bras-Goncalves RA, Pocard M, Formento JL, et al. Synergistic efficacy of 3n-butyrate and 5-fluorouracil in human colorectal cancer xenografts via modulation of DNA synthesis. Gastroenterology. 2001;120:874–88.
9. Bostick RM, Potter JD, Sellers TA, et al. Relation of calcium, vitamin D, and dairy food intake to incidence of colon cancer among older women. The Iowa Women's Health Study. Am J Epidemiol 1993;137:1302-17.
10. Zheng W, Anderson KE, Kushi LH, et al. A prospective cohort study of intake of calcium, vitamin D, and other micronutrients in relation to incidence of rectal cancer among postmenopausal women. Cancer Epidemiol Biomarkers Prev 1998;7:221-5.
11. Ishihara J, Inoue M, Iwasaki M, et al. Dietary calcium, vitamin D, and the risk of colorectal cancer. Am J Clin Nutr 2008;88:1576-83.
12. Martinez ME, Giovannucci EL, Colditz GA, et al. Calcium, vitamin D, and the occurrence of colorectal cancer among women. J Natl Cancer Inst 1996 ;88 :1375-82
13. Bischoff-Ferrari HA, Giovannucci E, Willett WC, et al. Estimation of optimal serum concentrations of 25- hydroxyvitamin D for multiple health outcomes. Am J Clin Nutr 2006;84:18-28.
14. Ng K, Scott JB, Drake BF, et al. Dose response to vitamin D supplementation in African Americans: results of a 4-arm, randomized, placebo-controlled trial. Am J Clin Nutr 2014;99:587-98.
15. Garland CF, Gorham ED, Mohr SB, et al. Vitamin D for cancer prevention: global perspective. Ann Epidemiol 2009;19:468-83.
16. Dinkova-Kostova AT, Kostov RV. Glucosinolates and isothiocyanates in health and disease. Trends Mol Med 2012;18:337-47.
17. Jeffery EH, Jarrell V. Cruciferous vegetables and cancer prevention. In: Wildman REC, editor. Handbook of Nutraceuticals and Functional Foods.Boca Raton: CRC Press; 2001. p. 169-91. Vallejo F, Tomas-Barberan F, Garcia-Viguera C. Health-promoting compounds in broccoli as influenced by refrigerated transport and retail sale period. J Agric Food Chem 2003 May 7;51(10):3029-34.
18. Hu R, Khor TO, et al. Cancer chemoprevention of intestinal polyposis in ApcMin/+ mice by sulforaphane, a natural product derived from cruciferous vegetable. Carcinogenesis 2006 May 4.
19. Brew CT, Aronchik I, et al. Indole-3-carbinol activates the ATM signaling pathway independent of DNA damage to stabilize p53 and induce G1 arrest of human mammary epithelial cells. Int J Cancer 2006 February 15;118(4):857-68.
20. Firestone GL, Bjeldanes LF. Indole-3-carbinol and 3-3'-diindolylmethane antiproliferative signaling pathways control cell-cycle gene transcription in human breast cancer cells by regulating promoter-Sp1 transcription factor interactions. J Nutr 2003 July;133(7 Suppl):2448S-55S.
21. Yanaka A, Fahey JW, Fukumoto A et al. (2009) Dietary Sulforaphane-Rich Broccoli Sprouts Reduce Colonization and Attenuate Gastritis in Helicobacter pylori-Infected Mice and Humans. Cancer Prevention Research 2, 353-360.
22. Song L, Thornalley PJ. Effect of storage, processing and cooking on glucosinolate content of Brassica vegetables. Food Chem Toxicol 2007 February;45(2):216-24.
23. S. Kim, D.P. Sandler, J. Galanko, C. Martin, R.S. Sandler, Intake of polyunsaturated fatty acids and distal large bowel cancer risk in whites and African Americans, Am. J. Epidemiol. 171 (2010) 969–979.
24. G.K. Pot, A. Geelen, E.M. van Heijningen, C.L. Siezen, H.J. van Kranen, E. Kampman, Opposing associations of serum n-3 and n-6 polyunsaturated fatty acids with colorectal adenoma risk: an endoscopy-based case-control study, Int. J. Cancer 123 (2008) 1974–1977.
25. Q. Huang, J. Wen, G. Chen, M. Ge, Y. Gao, X. Ye, et al., Omega-3 polyunsaturated fatty acids inhibited tumor growth via preventing the decrease of genomic DNA methylation in colorectal cancer rats, Nutr. Cancer 68 (2016) 113–119.
26. World Cancer Research Fund / American Institute for Cancer Research. Continuous Update Project Report. Food, Nutrition, Physical Activity, and the Prevention of Colorectal Cancer, 2011.
27. Wu AH, Paganini-Hill A, Ross RK, et al. Alcohol, physical activity and other risk factors for colorectal cancer: a prospective study. British journal of cancer 1987;55:687-94.
Order the nutrients mentioned in this article

Broccoli Sulforaphane Glucosinolate is formulated from a standardised extract of broccoli (Brassica oleracea).
www.supersmart.comFurther reading
10-10-2016
In India, turmeric is used to treat a wide variety of ailments including gastrointestinal problems, inflammation, headaches, infections and colds. It is turmeric’s curcuminoid content,...
Read more22-02-2017
Louis XIV famously suffered from severe constipation and his doctors would regularly ask him: ”Comment allez-vous (How are you)?”, when what they actually meant was:...
Read more29-01-2018
Every year, more than 750,000 people die from stomach cancer, one of the five most deadly forms of the disease. The main culprit is a...
Read more© 1997-2025 Fondation pour le Libre Choix
All rights reserved
All rights reserved
Free
Thank you for visiting our site. Before you go
REGISTER WITHClub SuperSmart
And take advantage
of exclusive benefits:
of exclusive benefits:
- Free: our weekly science-based newsletter "Nutranews"
- Special offers for club members only





















